Mental health challenges now touch more than a billion lives worldwide, and adolescents sit at the most vulnerable crossroads of […]
Cannabis Derivatives Show Promise as Future Treatments for Ovarian Cancer
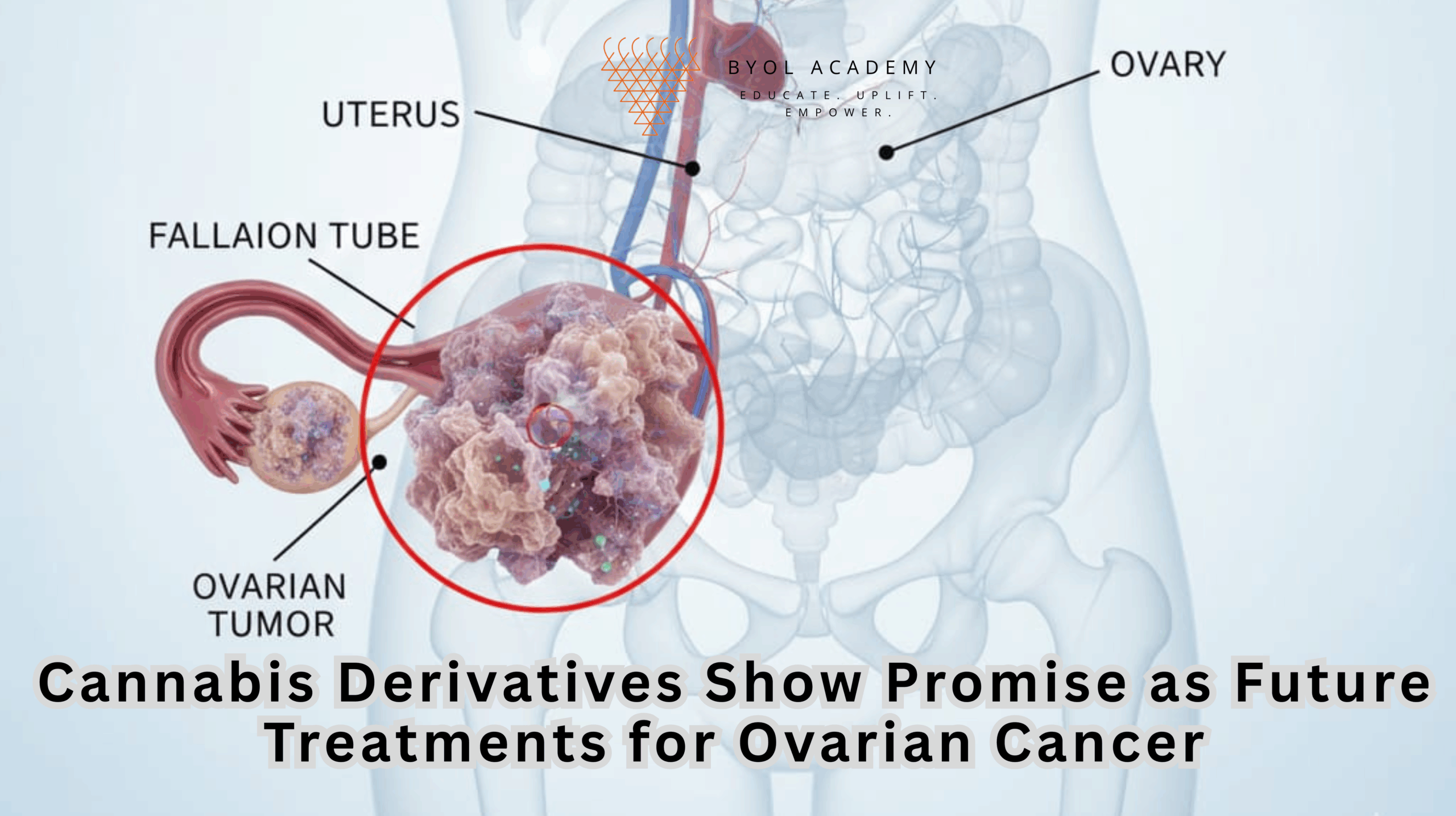
Ovarian cancer sits at a grim crossroads of modern oncology. It is not the most common cancer in women, yet it is the most lethal among gynecological malignancies, a consequence of biology, timing, and silence. Early disease rarely announces itself clearly, effective screening tools remain elusive, and by the time symptoms demand attention, the cancer has often advanced. Surgery and chemotherapy have improved survival, but relapse is common, and recurrent tumors frequently learn how to survive the very drugs designed to destroy them. This cycle of late detection, temporary control, and treatment resistance has forced researchers to look beyond conventional therapeutic boundaries toward biologically credible but less traditional solutions.
One such direction has emerged from an unlikely source: Cannabis sativa. Long associated with neurological and pain-related research, cannabis has increasingly drawn attention for its molecular interactions with cancer biology.
A recent study published in Frontiers in Pharmacology has strengthened this scientific shift. Investigating two of the plant’s most studied compounds, cannabidiol (CBD) and delta-9-tetrahydrocannabinol (THC), researchers found that both exert notable anti-cancer effects on ovarian cancer cells in controlled laboratory settings. Crucially, these effects were not limited to tumors that remain responsive to standard chemotherapy. The compounds also suppressed growth in ovarian cancer cells resistant to platinum-based drugs, a clinical scenario that typically signals limited treatment options and poor prognosis.
Together, these findings suggest that cannabis-derived molecules may interact with ovarian cancer through mechanisms distinct from conventional therapies, opening a new conceptual space in the search for treatments capable of confronting both disease progression and therapeutic resistance.
The clinical burden of ovarian cancer
Ovarian cancer is often described as a “silent killer.” Early-stage disease typically produces vague symptoms, such as bloating, abdominal discomfort, or fatigue that are easily overlooked. As a result, many patients are diagnosed at advanced stages, when the cancer has already spread beyond the ovaries.
Standard treatment consists of cytoreductive surgery followed by platinum-based chemotherapy. Although many patients initially respond, recurrence is common, and recurrent tumors frequently develop resistance to chemotherapy. Available second-line treatments often provide limited benefit and are associated with significant toxicity. As Dr. Siyao Tong of Khon Kaen University, lead author of the study, noted, ovarian cancer is characterized by “late diagnosis, high recurrence rates, and limited effective treatment options,” highlighting the urgent need for novel, more effective therapies.
Why investigate cannabis-derived compounds?
Cannabis contains a diverse array of biologically active molecules known as cannabinoids. Among these, CBD and THC are the most extensively studied. CBD is non-psychoactive and has shown anti-inflammatory, anti-proliferative, and neuroprotective effects in various disease models. THC, although psychoactive, has also demonstrated anti-tumor activity in multiple cancers.
Previous studies have suggested that cannabinoids can influence key cancer-related processes, including cell proliferation, apoptosis (programmed cell death), migration, angiogenesis, and immune signaling. However, evidence specific to ovarian cancer, especially chemotherapy-resistant disease has been limited. This study directly addressed that gap using a systematic and mechanistic approach.
Study design and experimental approach
The researchers examined the effects of CBD and THC on two distinct ovarian cancer cell lines: one sensitive to platinum-based chemotherapy and one resistant to it. This distinction is clinically critical, as platinum resistance is associated with poor prognosis and limited therapeutic options.
Cancer cells were treated with CBD alone, THC alone, and a combination of both compounds. A line of healthy cells was also included to assess whether these compounds caused non-specific toxicity.
The study evaluated multiple cancer-relevant outcomes, including cell survival, colony formation, migration, and intracellular signaling pathways associated with tumor growth and drug resistance.
Suppression of cancer cell growth and survival
Both CBD and THC significantly reduced the ability of ovarian cancer cells to survive and proliferate. Treated cancer cells formed fewer and smaller colonies, indicating a marked suppression of growth. While each compound alone demonstrated anti-cancer activity, the most pronounced effects occurred when CBD and THC were used together.
The combination therapy, particularly at a 1:1 ratio was substantially more effective than either compound alone. Notably, this enhanced effect was observed in both chemotherapy-sensitive and chemotherapy-resistant cell lines, suggesting that the cannabinoids act through mechanisms distinct from those targeted by platinum-based drugs.
Although neither compound alone caused extensive cancer cell death, their combination induced significantly higher levels of growth inhibition and cell death, pointing toward a synergistic interaction.
Inhibition of migration and metastatic potential
Beyond reducing proliferation, CBD and THC also impaired cancer cell migration. This finding is especially important because ovarian cancer mortality is driven largely by metastasis rather than the primary tumor. The ability of cancer cells to migrate within the abdominal cavity enables widespread disease that is difficult to control surgically or pharmacologically.
By limiting migration, cannabinoid-based treatments could potentially slow disease spread and reduce metastatic burden, an effect that could translate into meaningful clinical benefit.
Selectivity and reduced toxicity
A striking and encouraging observation was the minimal effect of CBD and THC on healthy cells. Unlike many chemotherapeutic agents, which damage both cancerous and normal rapidly dividing cells, the cannabinoid treatments appeared relatively selective for cancer cells.
If this selectivity is maintained in animal models and human studies, cannabinoid-based therapies could offer a more favorable toxicity profile. Reduced toxicity would not only improve quality of life but also allow longer treatment durations and combination with other therapies.
Molecular mechanisms: targeting cancer survival pathways
To understand how CBD and THC exert their anti-cancer effects, the researchers examined intracellular signaling pathways. Particular attention was given to the PI3K/AKT/mTOR pathway, a central regulator of cell growth, metabolism, and survival.
This pathway is frequently over activated in ovarian cancer and is strongly associated with tumor progression and resistance to chemotherapy. The study found that CBD and THC appeared to restore more normal regulation of this pathway, reducing aberrant survival signaling. This mechanistic insight strengthens the biological plausibility of cannabinoids as targeted anti-cancer agents rather than non-specific toxins.
Implications for ovarian cancer treatment
The findings have several important implications. First, they suggest that cannabinoid-based therapies could play a role in treating chemotherapy-resistant ovarian cancer, a setting where therapeutic options are currently limited. Second, their apparent selectivity raises the possibility of treatments that are both effective and better tolerated than existing regimens.
The ability to inhibit cell migration also points toward a potential role in controlling metastatic disease, which is responsible for most ovarian cancer–related deaths.
Implications for combination therapy
The enhanced effect observed with combined CBD and THC highlights the importance of combination strategies in modern oncology. Cannabinoids may function best not as standalone drugs but as adjunct therapies, potentially sensitizing tumors to chemotherapy, allowing lower drug doses, or targeting complementary survival pathways.
Such combination approaches align with the broader shift toward multi-target, precision-based cancer therapy.
Future directions and challenges
Despite their promise, these findings remain preliminary. All experiments were conducted in vitro, and laboratory results do not always translate directly to living organisms. Critical next steps include in vivo studies to assess efficacy, safety, dosing, and drug distribution, followed by carefully designed clinical trials.
Further research is also needed to identify which ovarian cancer subtypes are most likely to respond, potentially through biomarkers such as cannabinoid receptor expression or pathway activation profiles. Additionally, regulatory and legal considerations surrounding cannabinoid-based medicines will influence how quickly such therapies can move toward clinical use.
Conclusion
Cannabis-derived compounds are not a cure for ovarian cancer, nor are they ready for immediate clinical application. However, this research provides compelling evidence that CBD and THC particularly in combination, can disrupt key processes underlying ovarian cancer growth, spread, and drug resistance.
By grounding their effects in well-defined molecular pathways and demonstrating activity against resistant cancer cells with minimal harm to healthy cells, this study positions cannabinoids as serious candidates for future drug development. With rigorous follow-up research, cannabis derivatives may one day contribute to safer, more effective treatment strategies for one of the most challenging cancers in women’s health.