For a long time, cricket has been seen as a religion in India. But for decades, this devotion was mostly […]
Arsenic Exposure Linked to Rising Cases of MASLD: New Study Reveals a Hidden Connection
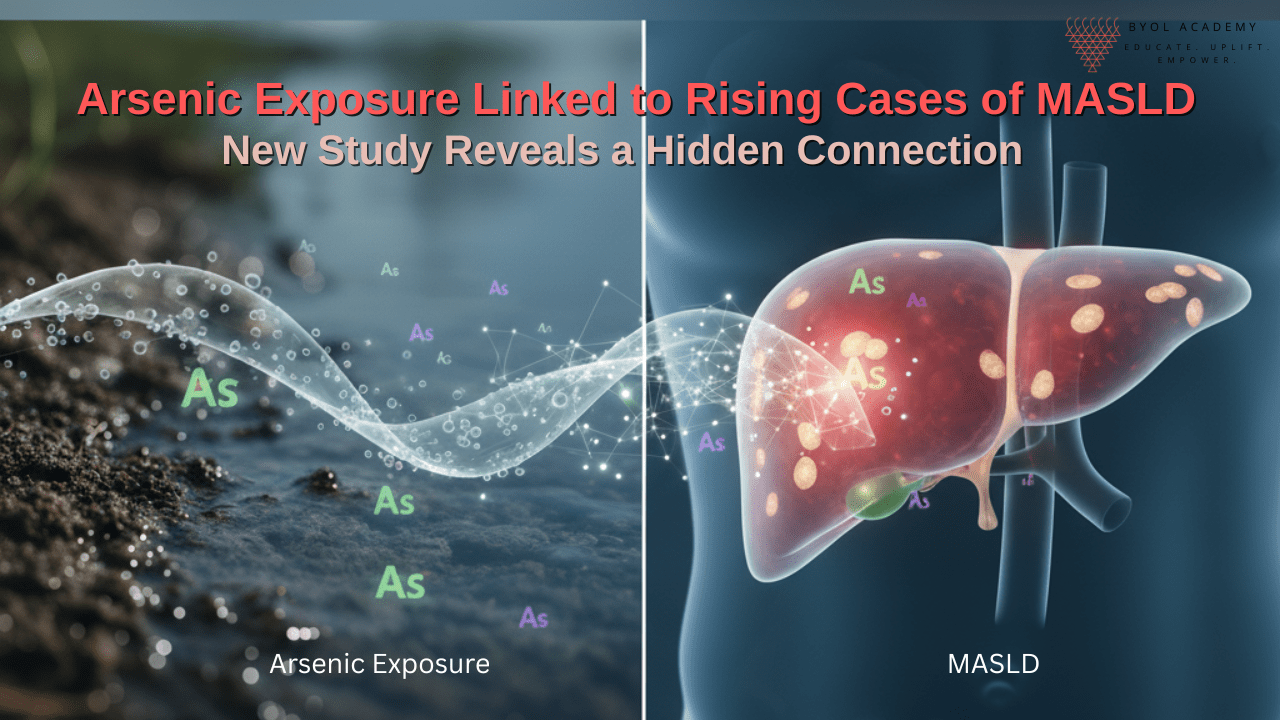
While doctors treat MASLD as a metabolic disorder, researchers are uncovering an invisible partner in crime – arsenic exposure. Found in contaminated groundwater and food, this silent toxin interferes with insulin signaling, mitochondrial function, and fat metabolism, pushing the liver toward disease.
It’s time to view MASLD not only as a nutritional disorder but as a toxicological one – where environment and metabolism collide.
The future of liver health might depend as much on clean water as on healthy food.
A recent analysis using National Health and Nutrition Examination Survey (NHANES, 2011–2020) data suggests that arsenic exposure may significantly increase the risk of MASLD in humans.
The Study at a Glance
Researchers analyzed data from 6,386 adults across the United States, linking urinary inorganic arsenic levels with liver health indicators. Mortality data were obtained from the National Death Index. Using weighted linear regression and chi-squared analysis, they evaluated how arsenic exposure related to MASLD and its associated risk factors.
Key Findings
Higher Arsenic, Higher Liver Risk:
Average urinary arsenic levels were 5.92 µg/L in people with MASLD compared to 5.59 µg/L in those without.
Liver Enzyme Trends:
Levels of alanine aminotransferase (ALT) -a key marker of liver injury – rose consistently with increasing arsenic levels, suggesting a dose-dependent relationship.
Demographic Differences:
- MASLD was more common in women (57.9%) than men (47.6%).
- The average age of individuals with MASLD was 49.9 years, compared to 46.9 years in those without.
- The condition was most prevalent among White participants, but showed a rising trend among Hispanic populations, especially Mexican Americans, who accounted for 12.6% of MASLD cases (p < 0.001).
Socioeconomic Factors:
The income-to-poverty ratio and body mass index (BMI) increased significantly with higher arsenic exposure, while education level did not show a clear association.
Strong Statistical Link:
Individuals in the highest arsenic exposure group had a 32% greater risk of MASLD compared to those in the lowest exposure group (p-trend- 0.002).
After adjusting for other factors, this risk rose to 55% higher odds (Odds Ratio 1.55; 95% CI: 1.19–2.03; p-trend < 0.001).
Arsenic: A Silent Global Health Threat
Arsenic, a toxic metalloid found in groundwater, industrial waste, pesticides, and foods like rice and seafood, poses a major health risk in India, Bangladesh, Nepal, the U.S., and Latin America.
Long-term exposure is linked to skin disease, heart problems, diabetes, cancers, and growing evidence suggests it also contributes to metabolic and liver disorders such as MASLD.
Arsenic and MASLD: Understanding the Biological Connection
The liver is the primary site for arsenic metabolism and detoxification. Chronic arsenic exposure may trigger several pathophysiological changes that increase the risk of MASLD:
1. Oxidative Stress:
Arsenic induces reactive oxygen species (ROS), damaging hepatocytes and promoting lipid accumulation.
2. Mitochondrial Dysfunction:
It impairs mitochondrial enzymes, leading to disrupted fatty acid oxidation and hepatic steatosis.
3. Insulin Resistance:
Chronic arsenic exposure interferes with insulin signaling, a major driver of MASLD pathogenesis.
4. Epigenetic Modifications:
Arsenic can alter DNA methylation patterns in genes regulating lipid metabolism, inflammation, and fibrosis.
5. Inflammatory Cascade Activation:
Upregulation of inflammatory cytokines such as TNF-α and IL-6 leads to hepatocellular inflammation and fibrosis progression.
A Growing Environmental Health Concern
These findings highlight an often-overlooked factor in the global surge of MASLD – environmental contamination. While obesity and metabolic syndrome remain critical drivers, toxic exposures like arsenic could be silently amplifying the problem.
The study’s lead data suggest that even moderate levels of arsenic exposure may worsen liver health, especially in vulnerable populations with metabolic risk factors.
Public Health Implications
The results underline an urgent need for:
- Regular monitoring of arsenic in drinking water and food sources.
- Public awareness campaigns about environmental toxins and liver health.
- Integration of environmental exposure screening into metabolic and liver disease prevention programs.
- Addressing arsenic exposure is not only an environmental issue – it’s a public health priority with potential to reduce the growing burden of liver disease.
Conclusion
This large-scale analysis offers strong evidence that arsenic exposure is independently associated with a higher likelihood of MASLD. As liver disease continues to rise globally, tackling environmental toxins like arsenic could become a crucial step in improving metabolic and liver health.
The message is clear: protecting our water, food, and environment may be as vital to liver health as managing diet and exercise.
References-
- Li W, Jiang X, Qian H, Li X, Su J, Zhang G, Li X. Associations of arsenic exposure with liver injury in US adults: NHANES 2003–2018. Environmental Science and Pollution Research International. 2023 Apr;30(16):48260–48269. doi:10.1007/s11356-023-25540-5. (Cross-sectional NHANES analysis showing positive associations between urinary arsenic/DMA and liver injury biomarkers.)
- Liu Y, Li W, Zhang J, Yan Y, Zhou Q, Liu Q, et al. Associations of arsenic exposure and arsenic metabolism with the risk of non-alcoholic fatty liver disease. International Journal of Hygiene and Environmental Health. 2024 Apr;257:114342. doi:10.1016/j.ijheh.2024.114342. (Case-control / population study reporting associations between inorganic arsenic, arsenic methylation patterns, and NAFLD.)
- World Health Organization (WHO). Arsenic – Fact sheet. WHO Newsroom, Fact sheets. 2022 (updated page; consult latest online). Available from: https://www.who.int/news-room/fact-sheets/detail/arsenic. Accessed 30 Oct 2025. (Authoritative summary of exposure sources, health effects, and priorities for control.)
- Chen J, Zhong Y, Liu X, Wang Z, Chen J, Song B, et al. Evaluation of the effects of three arsenolipids on liver damage: element imbalance and oxidative damage. eFood. 2023;4(4):e99. doi:10.1002/efd2.99. (Experimental in-vivo study: short-term arsenolipid exposure in mice caused hepatic damage via disruption of antioxidant enzymes, elemental imbalance and oxidative stress – supports mechanisms of arsenic-induced hepatic lipid/mitochondrial injury.)